The excitement surrounding the recent FDA approval for the first-ever gene therapy for cancer quickly drowned out concerns about serious side effects of this type of treatment. While the approval is indeed a momentous event for cancer patients and for medicine in general, it’s important for people to understand how this kind of treatment works and why it can go horribly awry.
The Novartis therapy, Kymriah, is based on a scientific advance commonly known as CAR T (that’s for chimeric antigen receptor T cells, but there won’t be a quiz later). What its discovery could mean for patients appeared so astonishing in 2011 that many scientists in the field dropped everything to focus on its potential. To get access to this apparent miracle drug, it costs a cool $475,000.
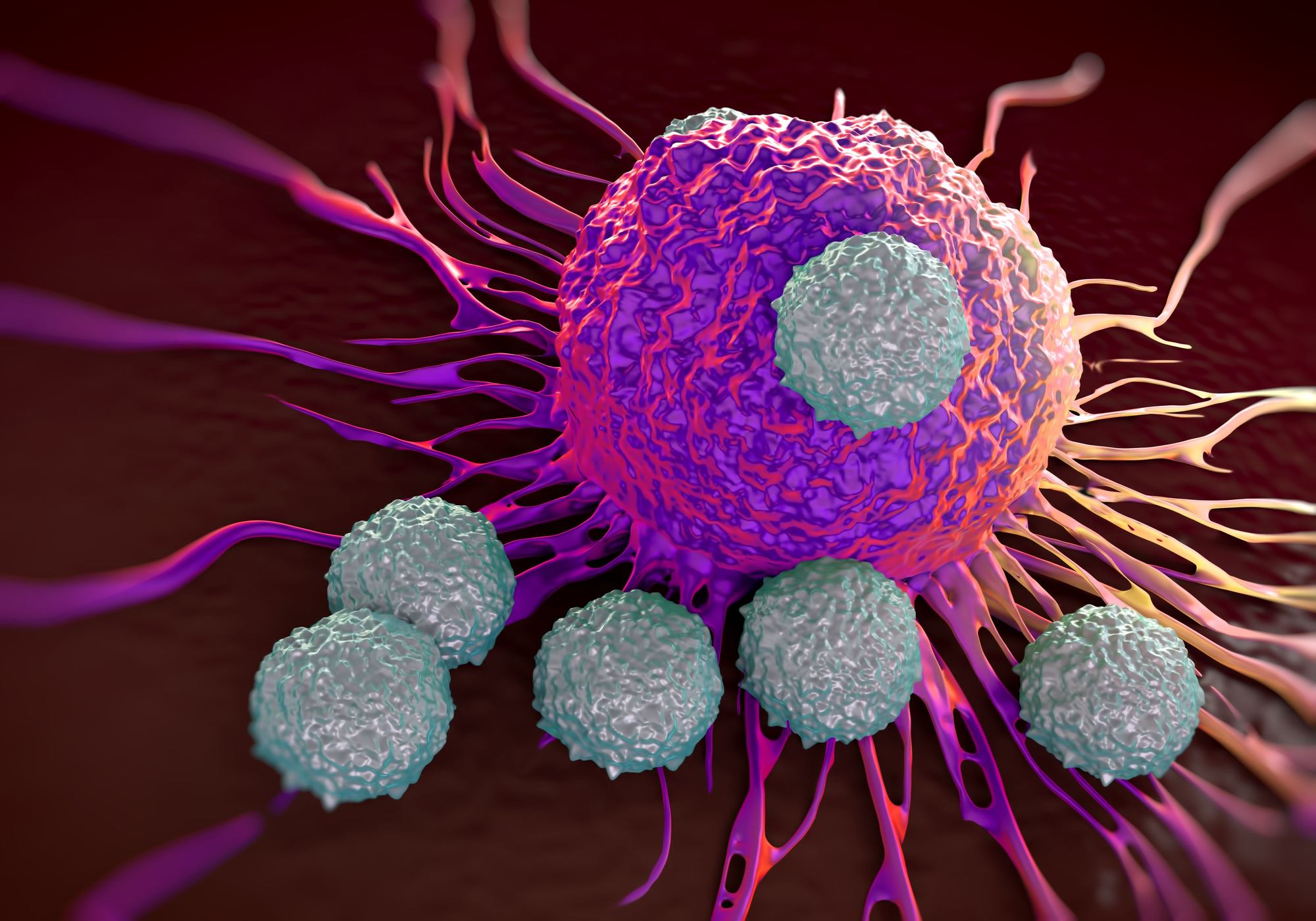
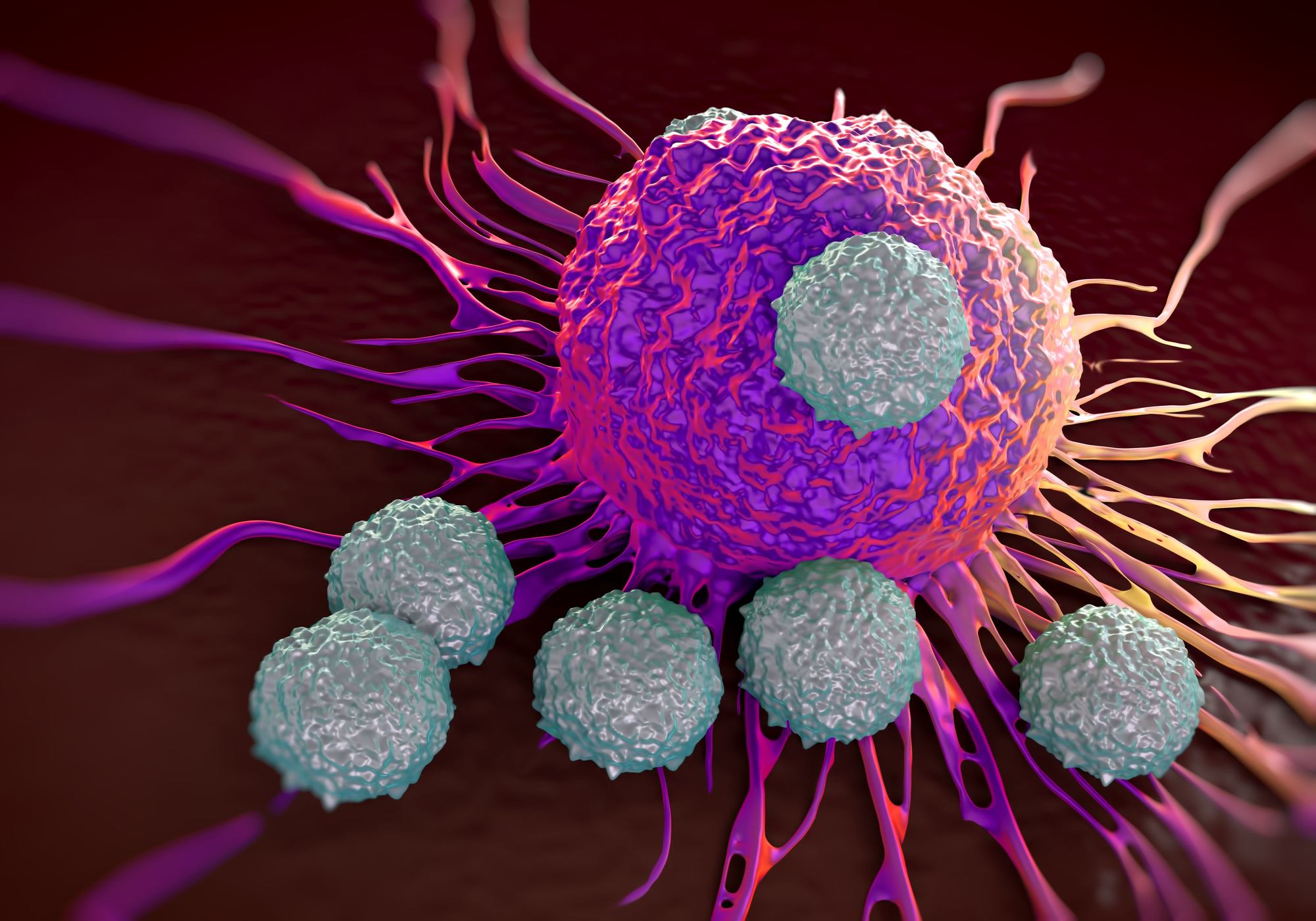
T cells are members of a person’s natural immune system brigade; in day-to-day life they defend against all sorts of pathogens. One of their responsibilities is distinguishing between cancer cells and healthy cells and mounting an attack when needed. The eureka moment of CAR T therapy occurred when scientists found they could harvest T cells from patients with cancer, modify them outside the body for a stronger response, and then re-introduce the souped-up cells to the patient. Because the cells came from the patient, they triggered no counterproductive immune response. And, stunningly, in many cases these cells went to work and destroyed even the most intransigent cancers in patients whose treatments had been unsuccessful with conventional therapies.
In a clinical trial, Novartis’s Kymriah treatment was given to 63 patients, all children or young adults whose cases of acute lymphoblastic leukemia had relapsed or proven resistant to standard treatments. These were effectively patients of last resort; rescuing even a few of them from their death sentences would have been impressive. Three months after treatment, 83 percent of patients were in remission. The panel of experts judging trial results for the FDA voted unanimously to approve the therapy for ALL patients 25 and younger.
And if that were the whole story, we’d be so busy dancing in the streets that I wouldn’t have time to write this article. But unfortunately there are some serious downsides to CAR T therapies. As you can imagine, planting revved-up immune cells in a patient is a little like unleashing an unstoppable monster. These cells are now programmed to attack things they would have otherwise left alone, and that response affects far more than cancer cells. In the Kymriah clinical trial, nearly half the patients developed serious infections and/or neurological conditions. Several patients needed dialysis or ventilators for a while, and many required long stays in intensive care.
But one adverse event was common to all patients, and was expected based on how the therapy works. Their overall immune system is drastically altered, and they consequently need to receive regular doses of immunoglobulins to shore it up—potentially for the rest of their lives. That can cost up to $10,000 per treatment and might be required every three to four weeks.
Clinical trials of other CAR T therapies have resulted in patient deaths, in the case of at least one drug so frequently that the trial was shut down. That kind of problem can be disastrous for a new type of treatment. Decades ago, a different but seemingly nascent gene-therapy field was completely derailed after a widely publicized patient death; it took years before scientists would go near it again.
FDA’s approval of Kymriah is a major step forward for cancer patients, for CAR T treatments, and for gene therapy in general. It will open the doors for more pharma companies and more investors to develop novel treatments, possibly expanding to other types of cancer or a broader range of patients. But in our eagerness to finally get the upper hand in the fight against cancer, we must not ignore the long-term risks these treatments entail. We just have to hope that future versions can become safer, more targeted, and less compromising to a patient’s overall health.
Seemingly Miraculous New Cancer Gene Therapy Brings Major Risks
A new FDA-approved cancer gene therapy called CAR T recently showed astonishing effectiveness against leukemia in seriously ill patients. Despite their poor prognosis, 83 percent responded to the treatment, and the cancer medical establishment was blown away. But even as we celebrate a genuine breakthrough, consider the very serious and long-lasting side effects.