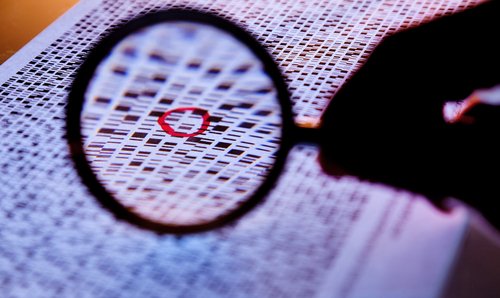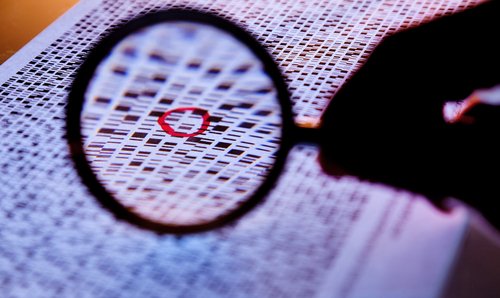
Affordable genome sequencing has brought with it a host of ethical debates. Who owns the data? Who can access the data? Should we sequence children? But the debate most likely to directly affect you in the next few years is this: what happens if your physician has your genome sequenced and finds something that she wasn’t looking for?
Let’s say, for example, your physician ordered a genome sequence for you to determine the cause of a chronic but fairly mild condition you have. When the results come back, there’s the answer to your current medical mystery, but there’s also a result telling the physician that you are at increased risk of hereditary cancer. That’s an incidental or secondary finding: medically important, but not what was being sought. The question is: do you want to know? Should you have the right to choose whether to see that result?
This question has reached full-battle proportions in the research and clinical communities. Some people advocate only returning the requested results. But others contend that if so-called incidental findings might eventually call for clinical intervention, they should be shared with the patient.
This discussion was on display at last month’s annual meeting of the American Society of Human Genetics (ACHG), which brought more than 6,000 scientists, clinicians, and genetic counselors together to hash out points of contention like this one. In a panel session on the subject, speakers argued passionately for both sides—and for more narrowly defined approaches that may serve as a sort of compromise.
This issue rose to a boiling point with an unexpectedly aggressive recommendation from the American College of Medical Genetics and Genomics (ACMG) earlier this year, which laid out a set of 57 genes that they said should be evaluated any time a physician orders a patient’s genome sequence or exome sequence (a smaller subset of the genome). This “duty to hunt,” as some people call it, was surprising—but what really got people’s attention was the part of the recommendation that said these findings should be shared even with patients who expressly do not want to know the results. (Genes related to diseases such as Alzheimer’s or Huntington’s, with no known medical treatment, are not on the list.)
“We recognize that this may be seen to violate existing ethical norms regarding the patient’s autonomy and ‘right not to know’ genetic risk information,” wrote the authors of the ACMG recommendations. “However … we felt that clinicians and laboratory personnel have a fiduciary duty to prevent harm by warning patients and their families about certain incidental findings and that this principle supersedes concerns about autonomy.”
Genes linked to hereditary breast and ovarian cancer are among the selected 57. In her presentation at the ASHG meeting, bioethicist Ellen Wright Clayton from Vanderbilt University argued that there are cases where even people who have cancer would be better off not knowing, noting that this applies even more for people who could be at increased genetic risk for one day developing cancer but are currently cancer-free. Scientists on the other side of the debate argue that not sharing such findings puts an undue burden on the researcher or physician who can’t help knowing what he may believe is a key piece of medical information about a patient, but is prevented by policy or patient preference not to reveal it.
Anecdotal evidence indicates that many physicians are not abiding by the ACMG recommendations, for the most part because they reject the notion that patient preference should be ignored. If there’s anything that was agreed on at the recent ASHG meeting, it was that there is a critical need for consensus in this new ethical quagmire: somebody needs to come up with a guideline that enough of the community supports before this rift gets even worse. The battle may be happening in scientific journals and at industry conferences, but the people likely to get caught in the crossfire are innocent bystanders: patients and consumers.
Should You Have the Right Not to Know Genetic Information?
Affordable genome sequencing has brought with it a host of ethical debates. Who owns the data? Who can access the data? Should we sequence children? But the debate most likely to directly affect you in the next few years is this: what happens if your physician has your genome sequenced and finds something that she wasn’t looking for?