When scientists first proposed the Human Genome Project in the 1980s, many expected, correctly, that understanding our genome would lead to what we now call precision medicine: the ability to tailor treatments and customize screening regimens for each patient. Nowhere have the benefits of this approach been felt more than in the area of oncology. Today’s targeted cancer treatments, along with genetic tests to identify people at increased risk of developing cancer, were largely built on the information gleaned from that first human genome sequence.
But there’s another opportunity that the Human Genome Project pioneers mostly didn’t foresee four decades ago — the ability to use noninvasive testing to diagnose cancer at the earliest stages. There are now many tests that can spot early biological hallmarks of a variety of types of cancer. Most of these tests are noninvasive, requiring just a sample of blood, urine, or stool.

That’s particularly good news, because many of the routine screening procedures we use to find cancer today are not working that well. In the past decade, for example, the U.S. Preventive Services Task Force reversed its position on mammograms for women aged 40 to 49; while the organization previously recommended the test for this age group, they now cite high rates of false positives and unnecessary biopsies as the reason why it’s better to wait until women are 50 to begin getting mammograms. The value of the widely-used prostate-specific antigen (PSA) test to detect prostate cancer has also been called into question for men in certain age groups or health states. And just recently, a large study of colonoscopy screening found that this common procedure was less effective than expected at detecting colorectal cancer and improving patient outcomes.
While noninvasive genomic and other tests for cancer are not intended to replace traditional screening methods, they provide a complementary approach that can reveal important molecular context to help make sense of other screening results.
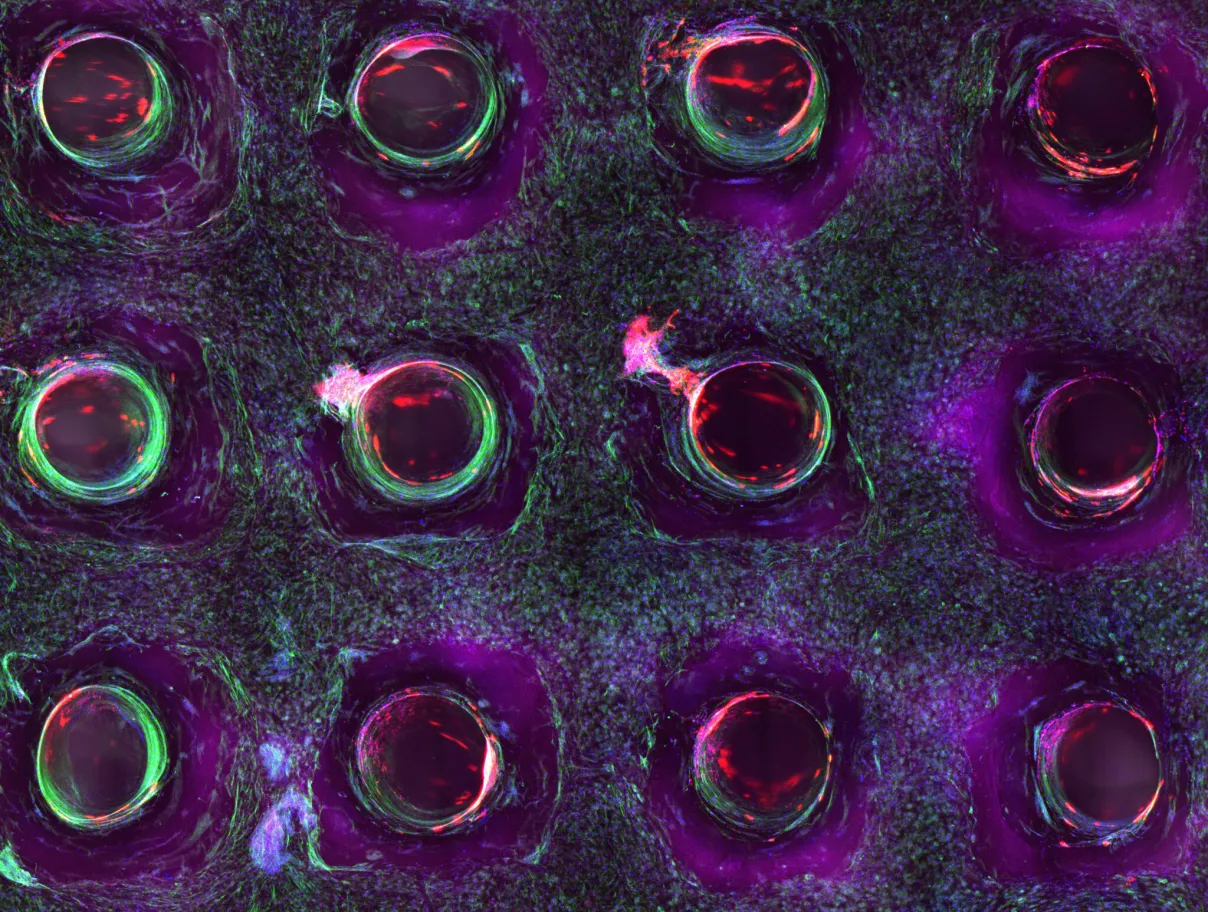
These molecular tests are based on highly sensitive technologies that can spot the smallest telltale traces of cancer. Some seek out tiny bits of genetic material shed by tumors; this cell-free DNA (also known as circulating tumor DNA) can be detected in a blood sample. Some of the earliest clinical studies of noninvasive prenatal screening — a technique that finds short bits of fetal DNA in a pregnant mother’s blood to learn about the health of her baby— unexpectedly detected this tumor-shed DNA in a small number of patients. The cancer was at such early stages that the mothers generally had no idea they were sick.
Other tests look for different materials originating from a tumor, such as exosomes. These tiny particles are part of a sophisticated cell-to-cell communication network in the body. Cells of all sorts pack up critical information in the form of DNA, RNA, and proteins, stuff it into a protective lipid layer, and shuttle the resulting exosome off to other cells in the body. Exosomes can be found in all biofluids; advanced technology can be used to decipher their molecular cargo, which in some cases can indicate the presence of cancer.

There is still much to be learned about all the different ways cancer might be detected early enough to give people the best chance at survival. For now, though, a whole generation of molecular tests promises to step in where traditional screening tools have fallen down.