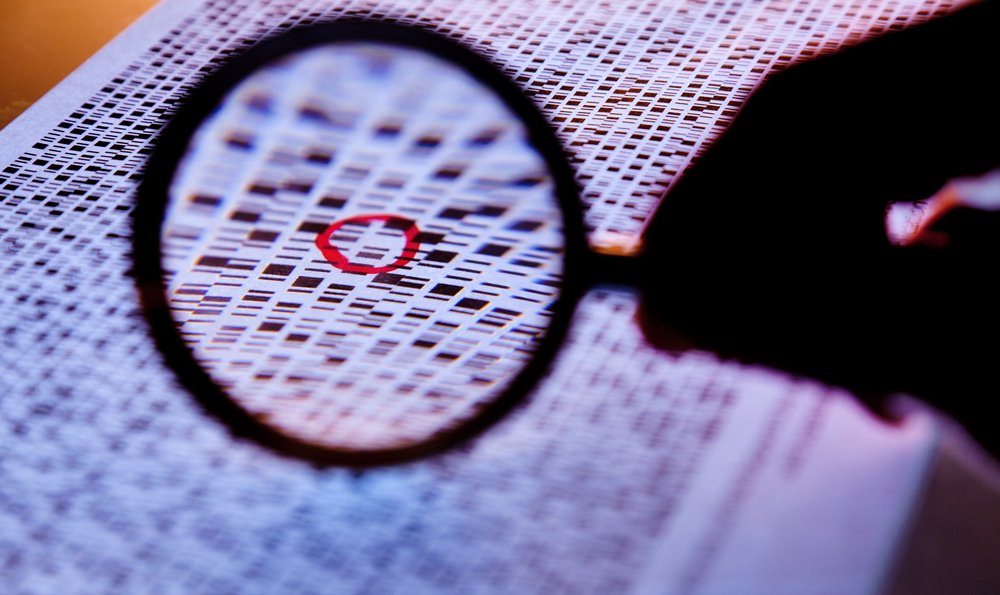
There’s growing debate in the biomedical community about the most valuable view of the human genome: a wide panoramic snapshot showing the whole thing, or a zoomed-in image of just where the action is. This is not just an academic discussion: the outcome will have significant implications in how patients are treated for a range of medical conditions.
The early days of genomics, dating back to the late ’80s and early ’90s, were all about the big picture. The Human Genome Project, which stirred up quite the controversy in its day, was a high-stakes bet that characterizing all 3 billion DNA base pairs in the human genome would be the best foundation for the nascent field and its long-term impact on medicine. At the time, even respected scientists argued that the project was a waste of money, and that research should focus only on the small percentage of the genome composed of active genes; the rest, they contended, was likely meaningless to how our bodies function. That view has since been disproven.
Having the full human genome sequence enabled researchers to look close-up at specific regions of interest to them, and learn that separate genetic regions often work together or interact to affect disease susceptibility. Today, that has led to a push to analyze more focused snippets of the genome—sometimes what is known as the exome, or all active genes, and other times pre-selected panels of genes known to play a role in a certain disease or biological function.
There are many reasons the targeted path has come into favor recently. In some cases we have learned enough to be confident that we don’t need a full genome to accurately detect the particular genes associated with a disease. Huntington’s disease is a good example: scientists have performed enough studies to know that this disease is caused by a single gene. Assessing someone’s risk of developing the disease is possible just by knowing the state of that lone gene.
Other benefits of targeted approaches include cost and turnaround time—at this point, it is less expensive and faster to look at a subset of genes than at the whole genome. Targeted peeks at DNA can also be far more sensitive than scanning a full genome; if a doctor is looking for one mutation, a targeted view is more likely to spot the presence or absence of that variant. This is akin to looking for a specific billboard while driving on a highway. For a whole genome, you’re driving on the highway at 65 miles per hour across 10 states. With a targeted approach, you already know the zip code of the billboard, so you drive at 10 miles per hour along just a small stretch of highway.
For these reasons, looking at a subset of the genome can be tremendously useful, particularly as hospitals begin to incorporate genomics routinely into clinical care. But there’s an important caveat: targeted approaches by definition will miss information. They are designed to take what we currently know and make it useful. We do not yet know all the genes that figure into breast cancer risk, for example, but we do know several of them. The targeted approach lets us put to use what we know and add to it as more genetic associations are uncovered.
Fragile X syndrome is a good illustration of the challenges of using limited information for patient care. Fragile X is known to be caused by a mutation in a single gene called FMR1. When this was first discovered, it was a huge advance, and doctors began testing for FMR1 mutations when Fragile X was the suspected diagnosis. But at the time, the way the disease was understood, a patient either had the mutation or didn’t, and therefore had the disease or didn’t. Today we know that the mutation happens in many copies—with enough mutations, a person will have Fragile X, but with fewer mutations, the person will still have certain symptoms and may develop related but less severe diseases. A simple yes/no analysis of the FMR1 mutation is not enough to provide that answer; more advanced genetic testing, and analysis of a broader region of DNA, is necessary to provide an accurate diagnosis.
This is a good reminder that we should not get lulled into believing that today’s highly targeted approaches are the ideal long-term solution. Our understanding of the human genome has improved greatly, but how each piece of DNA relates to biological function as a whole remains unclear. We must continue to invest heavily in elucidating the complex biological mechanisms underlying disease risk and development—and that means, among other things, ensuring that government agencies such as the National Institutes of Health and National Science Foundation are generously funded, even in tough economic times.
How to Look at Your Genome: Close-Up or Wide-Angle?
There’s growing debate in the biomedical community about the most valuable view of the human genome: a wide panoramic snapshot showing the whole thing, or a zoomed-in image of just where the action is. This is not just an academic discussion: the outcome will have significant implications in how patients are treated for a range of medical conditions.