Digital medicine is a hot topic in discussions about how to improve healthcare. It’s been driven by soaring investor interest, novel clinical goals, the push to implement precision medicine, and now the urgency of responding to the pandemic. In the past several years, one of the bellwethers of progress in this area has been efforts by Alphabet (otherwise known as Google). A recent presentation at the AGBT Precision Health conference from a leader of these initiatives shed light on how the internet giant views opportunities in digital health.
Robert Califf is head of clinical policy and strategy at Verily, an Alphabet subsidiary focused on optimizing the application of health information. He says digital medicine will be a fundamental element of precision medicine, which aims to get the right treatment to the right patient at the right time, partly through understanding their genetics. The digital component includes mining ever-larger data sets to find new insights and then delivering them back to physicians and patients in useful ways.

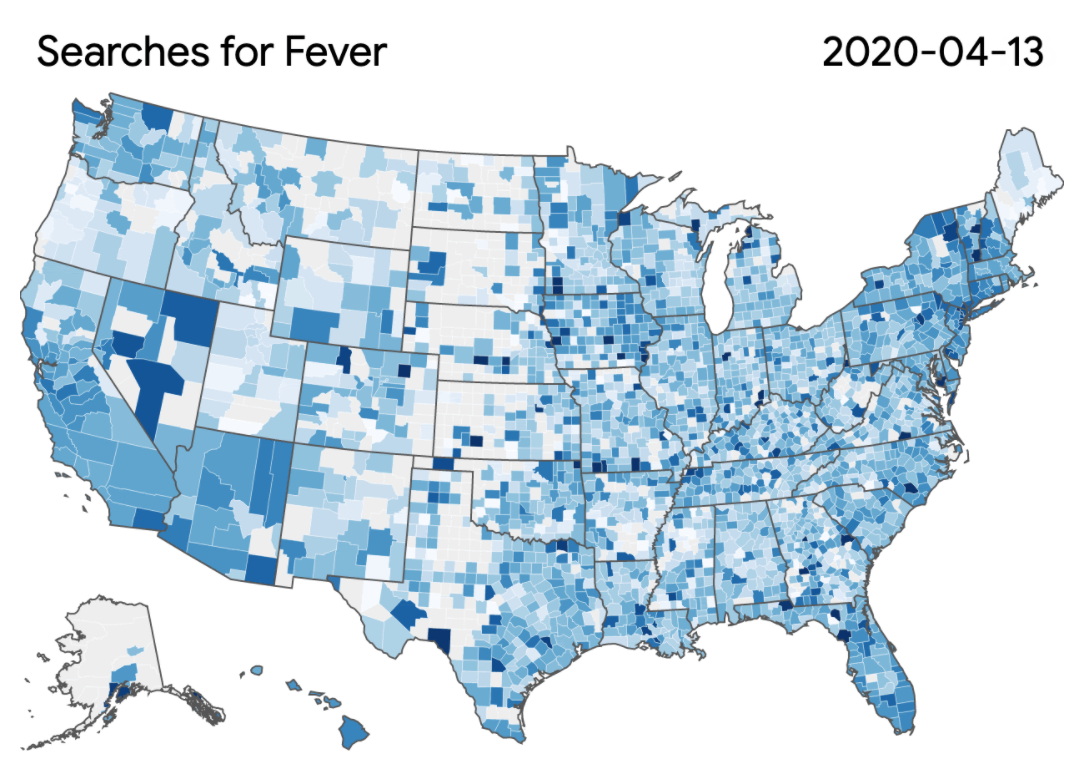
Google has a unique view of consumer health. According to Califf, the company estimates users of its search engine get 16.3 million results every 0.57 seconds. And 5% of queries are related to health. Tracking symptom-specific searches has proven helpful in public health, allowing Google to spot signs of flu outbreaks early. Such search data is also being used to learn more about the spread of the virus responsible for COVID-19.
Califf is excited about the potential to tackle some major population-scale health challenges by pairing that kind of data obtained from searches with existing statistics about health outcomes here in the U.S. He cited an example: compared to other high-income countries, he says, the U.S. has the lowest life expectancy. Historical data for a range of countries shows the U.S. was on par with its wealthy peers until the 1980s, when our trajectory branched off. “We have big disparities in both [healthcare] cost and life expectancy,” Califf said in the conference presentation. “The U.S. is a vast outlier.” One reason solving this problem has been so tricky is that life expectancy varies significantly across the country, and even within cities. In Washington, D.C., for example, there’s a 15-year difference in life expectancy depending on which Metro stop you live close to, Califf says.
Google and its related organizations have a number of goals for improving healthcare. For starters, Califf says, “we have to improve access to knowledge.” There are still many places in the country — including in major cities — where people lack broadband internet access. Overcoming this problem would allow providers of digital health solutions to reach everyone and tailor information to their specific needs and comprehension level. It would also facilitate what Califf refers to as “home inversion,” a model of care focused on giving people information at work or home, leaving clinical visits to focus on high-quality physician-patient interactions rather than having doctors distracted by entering patient information into electronic medical records and other forms of data-gathering.

Califf also hopes that digital health could help tackle some of the most difficult issues raised by complex and chronic conditions, for example depression. Despite the hundreds of millions of people around the world who have depression severe enough to need treatment — and despite strong response to treatment in the majority of those who do get help — it’s estimated that about half of people with depression go undiagnosed and untreated. Since many of those people run internet searches about their symptoms, Google has begun offering presenting search users with a clinically-validated patient health questionnaire designed to screen for depression.
Califf offered other examples of Google’s digital health efforts: it is working with Johnson & Johnson on a digital surgery platform that would allow experts to scrub in from a remote location or provide in-person doctors real-time guidance by loading data from hundreds of similar procedures; helping the Federal Department of Veterans Affairs healthcare system predict kidney injury and treat patients earlier than is possible with conventional methods; and Project Baseline, which aims to collect comprehensive data to map human health and determine the ways that wellness turns into disease in the real world. (Anyone can join the project and volunteer to participate in studies.)
In the earliest days of digital health, some experts believed this field would be doomed by unreliable data, especially when it was reported by patients themselves. But Califf seems unfazed. Even when data isn’t great, he says, “if you have enough data, you can make pretty good predictions.”